Understanding Parotidectomy

At Aglow ENT Centre, we understand that surgery can be intimidating. However, for patients with parotid gland tumours, surgery is likely necessary to remove them safely and prevent their spread.
What is a Parotidectomy and When is it Needed?
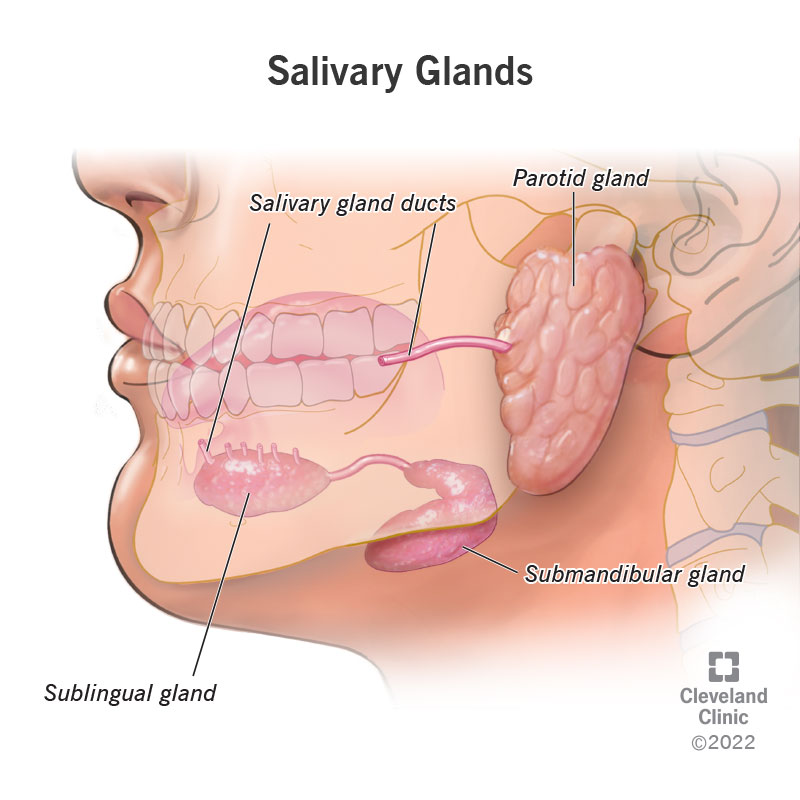
Parotidectomy (parotid gland tumour surgery) is performed in Singapore by ENT specialists as a specialised surgical procedure aimed at removing all or part of the parotid gland. The parotid gland is one of the major salivary glands located near the ear and extending down to the area beneath the jawline. Each individual has two parotid glands on each side of the face, which are important for producing saliva that aids digestion and maintains oral health.
When tumours, chronic infections, or other medical conditions affect this gland, you will be referred to a head and neck surgeon. Indicative symptoms may include visible lumps that grow in size in the head and neck area, pain, dry mouth, difficulty swallowing, or numbness in the facial area. Your surgeon may recommend one of two types of surgery based on your condition: a total parotidectomy or a superficial (partial) parotidectomy. The choice depends on how the parotid gland is positioned in relation to the facial nerve. This nerve runs through the gland, dividing it into two sections: the superficial lobe (above the nerve) and the deep lobe (below the nerve).
- Superficial (Partial) Parotidectomy: The surgery involves removing the superficial lobe of the parotid gland.
- Total Parotidectomy: The surgery involves removing the deep lobe only or both the deep and superficial lobes of the parotid gland.
Parotidectomy is performed under general anaesthesia, and patients may choose to go home the same day after surgery.
Who Can Perform Parotidectomy?
Parotidectomy, also commonly referred to as salivary gland tumour removal, is performed by head and neck surgeons. Given the intricate positioning of the facial nerve and parotid gland, it is imperative for patients to seek qualified and reliable surgeon for a parotidectomy. This helps to ensure minimal complications during the procedure. In Singapore, you can schedule an appointment at Aglow ENT Centre for an initial consultation. Our medical team is led by Dr Ker Liang who is an ENT head and neck surgeon with a specialisation in procedures such as parotidectomy.
Dr Ker Liang incorporates minimally invasive parotidectomy (micro-parotidectomy) into her practice when possible. With this approach, patients will likely experience reduced pain, minimal scarring, and swift recovery.
What to Expect
To help you or your loved ones prepare for a parotidectomy, here are some tips a parotid surgeon would recommend following.
Before the Surgery
Prior to surgery, there are key preparations that will facilitate the success of your operation.
These include:
- Scheduling an initial appointment with your surgeon to assess your current condition to ensure you are in good health for the procedure.
- A review of your medical history and medications will be conducted to minimise any potential complications.
- You may need to stop certain medications if your surgeon anticipates that they will interfere with your surgery.
- Your surgeon will request an imaging test, such as an MRI or a CT Scan. This will help your surgeon plan the most optimal way to remove your parotid gland with minimal risk to the rest of the facial area.
- A biopsy will be needed to determine whether your salivary gland tumour (if any) is cancerous. This is typically done using Fine-needle aspiration (FNA), where a thin needle is used to collect a sample.
- Once the surgery date is scheduled, you will be advised on when to fast and stop certain habits like smoking to minimise complications during the operation.
A parotidectomy may take 2 – 4 hours to complete on average. The actual duration of the surgery depends on the complexity of your condition. Patients with normal recovery may choose to leave on the same day. Therefore, you should arrange for someone to assist you in getting home.
During the Surgery
Once you are transferred to the operating theatre, you will be placed on general anaesthesia through an IV line. This ensures you are asleep throughout the procedure. Your parotid surgeon will begin the surgery by making an incision near the front of the ear and back, following the natural crease of your upper neck area. This incision pattern will help to hide your scars once you’ve healed. With the incision made, your surgeon can now gently remove the flap of skin to expose the parotid gland. During this step, your surgeon will take note of your facial nerve to avoid unnecessary contact with it. A facial nerve monitor will also be used to track the function of your facial nerves throughout the surgery. Depending on your condition, your surgeon will then remove part or all of your parotid gland and close the incision to complete the procedure.
After the Surgery
As soon as the procedure is completed, our medical team will transfer you to a recovery room where you will continue to be monitored. The team will check your blood pressure, heart rate, and other necessary vitals to ensure you are recovering well. After you wake up, your surgeon will come to check on you. This includes checking the function of your facial nerve after surgery. You may be asked to smile, close your eyes, or make other facial movements to ensure the nerve is not damaged.
It is normal to feel pain or numbness around the stitch area. You may also find that a neck drain has been placed in your wound site to remove excess blood and fluid after surgery – the drain functions to keep the area clean and free of possible infections. Your care team will inform you how to monitor the drain if you are sent home with it. You will still be able to eat, drink, and talk normally after the surgery, albeit with some sore discomfort that comes after the insertion of a breathing tube during surgery.
Once you are cleared to return home, here are some things to note on postoperative care:
- Diet: While there are no restrictions, you may want to consume soft food if your throat hurts.
- Medication: You will be provided antibiotics as part of your recovery plan.
- Wound Care: Make sure to keep your wound dry and clean by following your surgeon’s instructions on wound care. This will help reduce the risk of unwanted complications like an infection.
- Follow-up Appointment: Do not miss your next appointment. It is important for you to attend your follow-up appointments so that your surgeon can monitor your recovery progress.
The Benefits of Parotidectomy
Patients who have undergone a parotidectomy benefited in several ways, including:
- Preventing the escalation of tumour into cancer cells
- Preventing or minimise the spread of cancerous cells to other head and neck regions
- Preventing potential nerve damage from tumours that are left untreated
- Relieving symptoms for patients who encounter recurring infections.
What is the Success Rate of Parotidectomy?
Parotidectomy is considered to have a high success rate in terms of complete tumour removal and long-term management of symptoms. Specific percentages may vary based on the complexity of the case and the surgeon’s expertise.
What are the Potential Risks and Complications of Parotidectomy?
Common side effects following the surgical removal of the parotid gland include swelling, pain, and discomfort at the site of the surgery, which typically resolve within a few weeks. More serious complications, which can lead to facial paralysis or weakness, are less common. The side effects vary in severity and duration depending on the specifics of the surgery, the part of the gland removed, and the individual patient’s response.
When is a Parotidectomy Necessary?
A telltale sign that you may need a parotidectomy is when you notice visible lumps in your face or neck area, likely in your salivary glands (salivary gland lumps). The clinical term for this condition is known as parotitis.
These lumps are usually masses that can be caused by infections, cysts, salivary gland stones or tumours. In most cases, a parotidectomy is necessary when a tumour (benign or malignant) has been detected. Removal of the mass is crucial to prevent its growth or spread, which could cause serious complications.
If you have been diagnosed with a parotid salivary gland tumour, promptly consult a head and neck surgeon for the next course of action. At Aglow ENT Centre, you can book an appointment with our ENT head and neck surgeon, Dr Ker Liang, who is ready to support you with a personalised treatment plan to ensure your condition is under control and you recover successfully.
Dr Ker Liang handles ENT concerns from patients ranging from children to seniors. She provides comprehensive management covering non-surgical and surgical treatment approaches for ear, nose, and throat, as well as head and neck conditions.
Frequently Asked Questions (FAQs)
Can parotidectomy affect hearing?
A parotidectomy is unlikely to affect your hearing unless other complications occur.
How long is the recovery after parotidectomy?
Recovery after a parotidectomy usually takes 2 to 3 weeks for pain and swelling at the site of the surgery to subside. Dr Ker Liang at Aglow ENT Centre can provide personalised post-operative care and guidance.
How long does facial paralysis last after parotidectomy?
Facial paralysis may last up to a few weeks after surgery, but it will typically resolve on its own.
Will a parotidectomy leave a scar on my face?
ENT Head and Neck surgeons are trained to create an incision that will leave a minimally noticeable scar behind your ear or near your hairline.
Can parotid glands grow back after total removal?
No, parotid glands cannot grow back after being removed.
How long does it take for swelling to go down after parotidectomy?
The swelling usually goes down within 2 weeks after surgery.
What other conditions can be treated at Aglow ENT Centre?
Besides parotid gland tumours, Dr. Ker Liang treats various salivary gland disorders, swollen lymph nodes and thyroid lumps.
Medical Teaching
Assistant Professor Ker Liang has a passion for teaching and is an Assistant Professor with NUS Yong Loo Lin School of Medicine (YLLSOM). As the NUS-NUH Otolaryngology Department Undergraduate Medical Director, Dr Ker Liang supervises the training of medical students from YLLSOM, NUS. She is actively involved
in the training of postgraduate junior doctors and residents in the Head and Neck Surgery department. She was conferred with an Undergraduate Teaching Award by the National University Health System in 2016 for her outstanding efforts as an Otolaryngology educator.
Medical Teaching
Assistant Professor Ker Liang has a passion for teaching and is an Assistant Professor with NUS Yong Loo Lin School of Medicine (YLLSOM). As the NUS-NUH Otolaryngology Department Undergraduate Medical Director, Dr Ker Liang supervises the training of medical students from YLLSOM, NUS. She is actively involved
in the training of postgraduate junior doctors and residents in the Head and Neck Surgery department. She was conferred with an Undergraduate Teaching Award by the National University Health System in 2016 for her outstanding efforts as an Otolaryngology educator.



